Reese, Thomas J.; Padi-Adjirackor, Nana Addo; Griffith, Kevin N.; Steitz, Bryan; Patrick, Stephen W.; Leech, Ashley A.; Wiese, Andrew D.; Wright, Adam; Shah, Mauli V.; Ancker, Jessica S. “Comparative effectiveness of buprenorphine adherence with telemedicine Vs. in-person for rural and urban patients.” Journal of the American Pharmacists Association, 2025, 102318, https://doi.org/10.1016/j.japh.2024.102318.
During the COVID-19 pandemic, changes in policy allowed people to receive prescriptions for buprenorphine, a medication used to treat opioid addiction, through telemedicine without needing to visit a doctor in person. A new proposed rule, however, would limit the ability to receive buprenorphine prescriptions via telemedicine to just 30 days before requiring an in-person visit. This could disproportionately affect people living in rural areas, where access to healthcare may be more difficult. To understand the potential impact of this change, the study aimed to compare how well people followed their buprenorphine treatment when using telemedicine versus in-person visits, particularly focusing on rural versus urban patients.
The researchers analyzed electronic health records of patients who were prescribed buprenorphine between 2017 and 2022 at a large medical center. They looked at how regularly patients took their medication and whether there were any gaps in their treatment. The study included a total of 511 patients, with 3,302 in-person visits and 519 telemedicine visits. Overall, the study found no major differences in treatment adherence between telemedicine and in-person visits. However, for patients in rural areas, telemedicine visits led to better medication adherence, with fewer gaps in treatment and higher rates of taking the medication as prescribed, both in the short and long term.
In conclusion, the study suggests that telemedicine is a useful and effective option for prescribing buprenorphine, especially for patients living in rural areas. This finding is important for shaping future policies that aim to ensure continued access to this treatment, particularly for people who may face barriers to in-person visits.
Table 2
Unadjusted and adjusted association of visit type with buprenorphine adherence, stratified by rural and urban
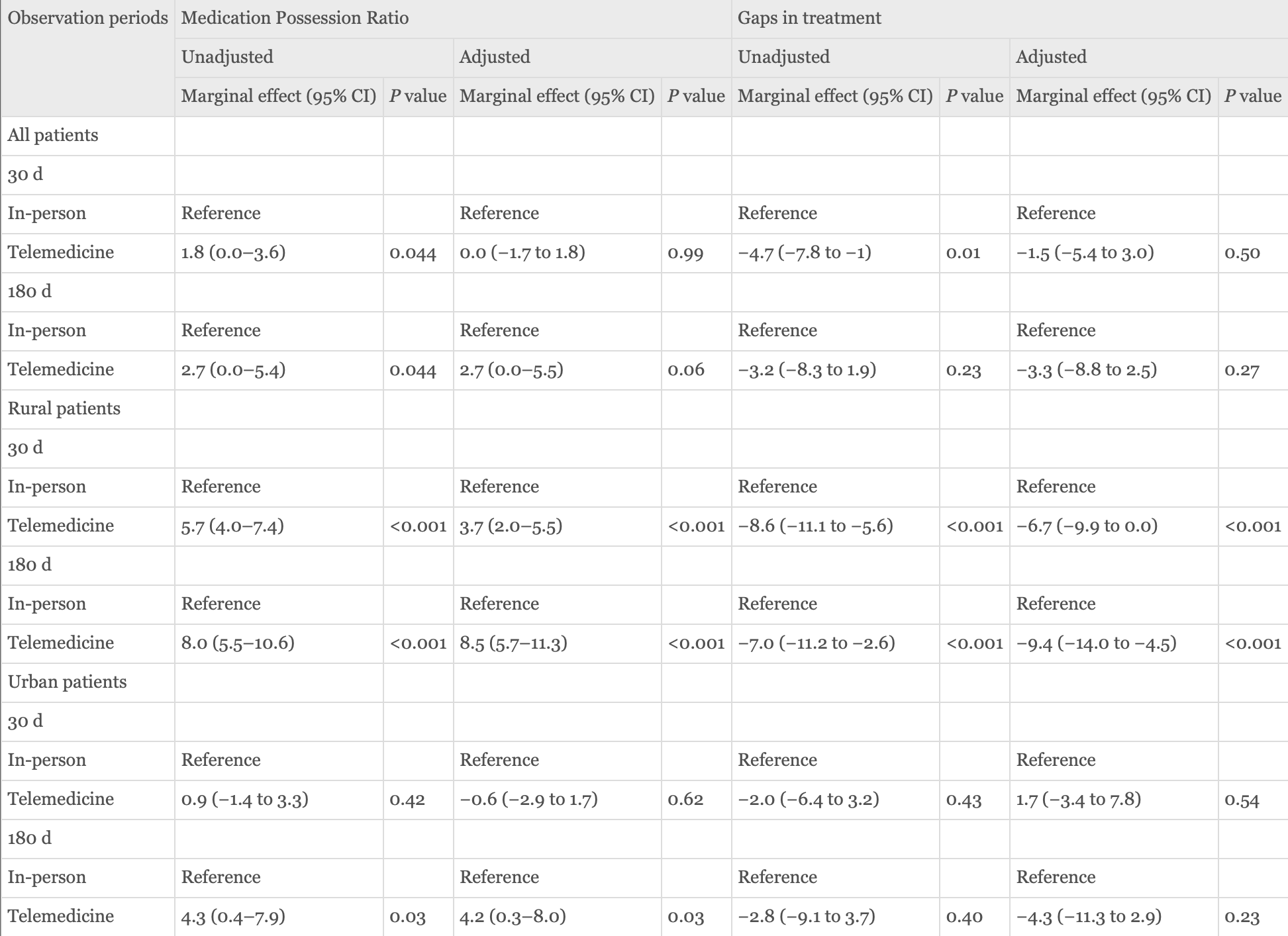
Note: Models adjusted for buprenorphine dose for the telemedicine or in-person visit, number of visits before the index visit, y of first prescription, and binary indicators for severe mental illnesses or comorbid substance use disorders including bipolar, depression, psychosis, anxiety, alcohol use disorder, cannabis use disorder, sedative use disorder, and stimulant use disorder documented during the study period. Additionally, we controlled for social determinants of health including percent unemployed and median household income for the patient’s ZIP code of residence (AHRQ, Social Determinants of Health Database).